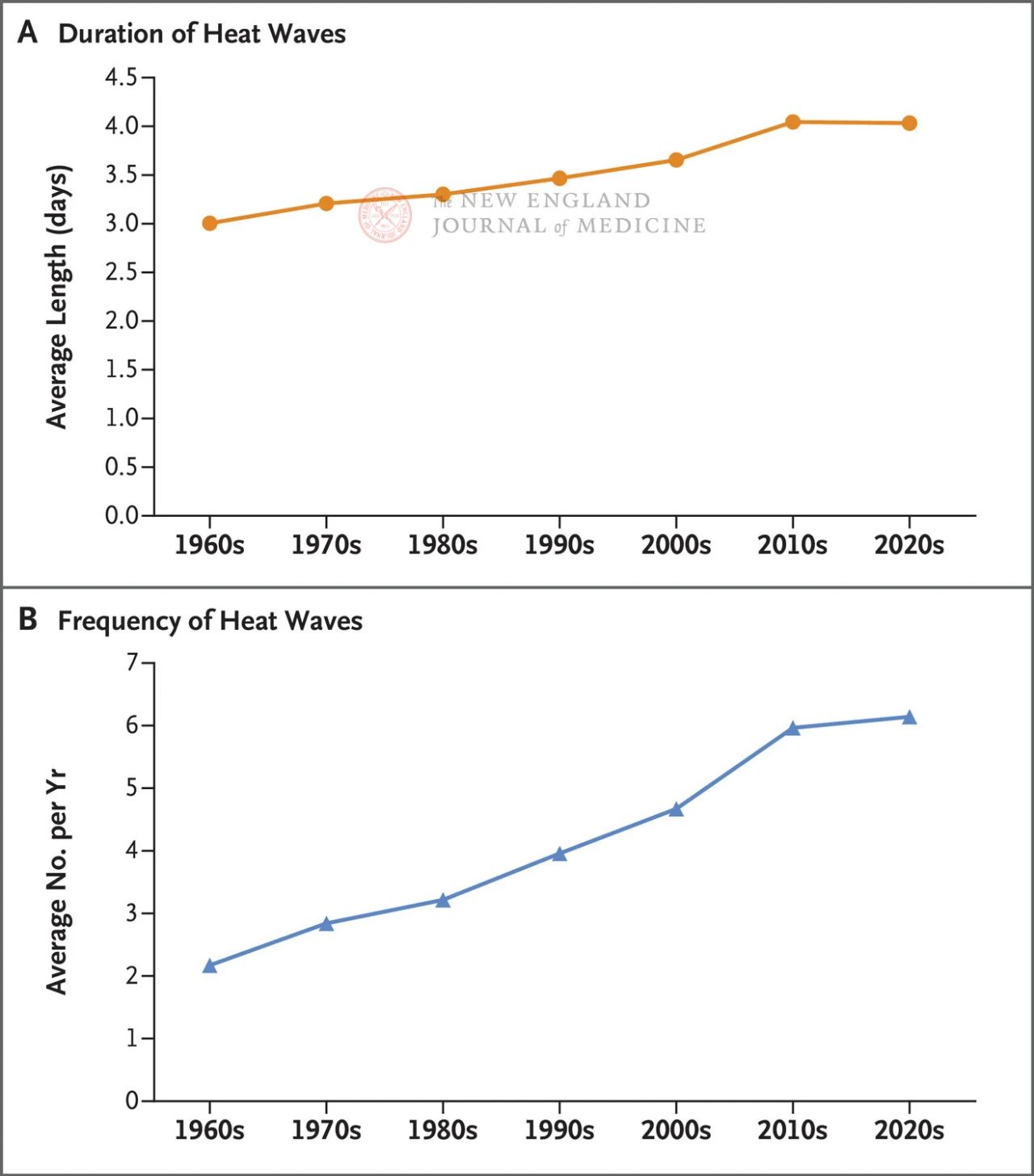
Entering the 21st century, the frequency, duration, and intensity of heat waves have significantly increased; On the 21st and 22nd of this month, the global temperature set a record high for two consecutive days. High temperatures can lead to a series of health risks such as heart and respiratory diseases, especially for sensitive populations such as the elderly, chronic diseases, and overweight. However, individual and group level preventive measures can effectively reduce the harm of high temperatures to health.
Since the Industrial Revolution, climate change has led to a global average temperature rise of 1.1 ° C. If greenhouse gas emissions are not significantly reduced, it is expected that the global average temperature will rise by 2.5-2.9 ° C by the end of this century. The Intergovernmental Panel on Climate Change (IPCC) has come to the clear conclusion that human activities, particularly the burning of fossil fuels, are the cause of overall warming in the atmosphere, land, and oceans.
Despite fluctuations, overall, the frequency and duration of extreme high temperatures are increasing, while extreme cold is decreasing. Composite events such as droughts or wildfires occurring simultaneously with heat waves have become increasingly common, and their frequency is expected to continue to increase.
A recent study shows that between 1991 and 2018, more than one-third of heat related deaths in 43 countries, including the United States, can be attributed to anthropogenic greenhouse gas emissions.
Understanding the widespread impact of extreme heat on health is crucial in guiding patient treatment and medical services, as well as developing more comprehensive strategies to mitigate and adapt to rising temperatures. This article summarizes epidemiological evidence on the health hazards caused by high temperatures, the excessive impact of high temperatures on vulnerable groups, and individual and group level protective measures aimed at mitigating these risks.
High temperature exposure and health risks
Both in the short and long term, exposure to high temperatures can seriously affect human health. High temperatures also indirectly affect health through environmental factors such as decreased quality and quantity of crops and water supply, as well as increased ground level ozone. The greatest impact of high temperatures on health occurs in extreme heat conditions, and the effects of temperatures exceeding historical norms on health are widely recognized.
Acute diseases related to high temperatures include heat rash (small blisters, papules, or pustules caused by blockage of sweat glands), heat cramps (painful involuntary muscle contractions caused by dehydration and electrolyte imbalance due to sweating), hot water swelling, heat syncope (usually associated with standing or changing posture for long periods of time in high temperatures, partly due to dehydration), heat exhaustion, and heatstroke. Heat exhaustion usually manifests as fatigue, weakness, dizziness, headache, profuse sweating, muscle spasms, and increased pulse; The patient’s core body temperature may increase, but their mental state is normal. Heat stroke refers to changes in central nervous system function when the core body temperature exceeds 40 ° C, which can progress to multiple organ failure and death.
Deviation from historical norms in temperature can seriously affect physiological tolerance and adaptability to high temperatures. Both absolute high temperatures (such as 37 ° C) and relative high temperatures (such as the 99th percentile calculated based on historical temperatures) can lead to high mortality rates during heatwaves. Even without extreme heat, hot weather can still cause harm to the human body.
Even with air conditioning and other factors that play a role in the adaptation process, we are approaching the limits of our physiological and social adaptability. The critical point includes the ability of existing power infrastructure to meet cooling needs in the long term, as well as the cost of expanding infrastructure to meet these needs.
High risk population
Both susceptibility (internal factors) and vulnerability (external factors) can alter the impact of high temperatures on health. Marginalized ethnic groups or low socioeconomic status are a key factor affecting risk, but other factors can also increase the risk of negative health impacts, including social isolation, extreme age, comorbidities, and medication use. Patients with heart, cerebrovascular, respiratory or kidney diseases, diabetes and dementia, as well as patients taking diuretics, antihypertensive drugs, other cardiovascular drugs, some psychotropic drugs, antihistamines and other drugs, will have an increased risk of hyperthermia related diseases.
Future needs and directions
It is necessary to conduct further research to understand the benefits of individual and community level heatstroke prevention and cooling measures, as many measures have synergistic benefits, such as parks and other green spaces that can increase sports activities, improve mental health, and social cohesion. It is necessary to strengthen the standard reporting of heat related injuries, including the International Classification of Diseases (ICD) codes, to reflect the indirect effects of high temperatures on health, rather than just the direct effects.
There is currently no universally accepted definition for deaths related to high temperatures. Clear and accurate statistics on heat related diseases and deaths can help communities and policy makers prioritize the health burden associated with high temperatures and develop solutions. In addition, longitudinal cohort studies are needed to better determine the different impacts of high temperatures on health based on the characteristics of different regions and populations, as well as the time trends of adaptation.
It is necessary to conduct multi sectoral research to better understand the direct and indirect impacts of climate change on health and identify effective strategies to enhance resilience, such as water and sanitation systems, energy, transportation, agriculture, and urban planning. Special attention should be paid to the highest risk groups (such as communities of color, low-income populations, and individuals belonging to different high-risk groups), and effective adaptation strategies should be developed.
Conclusion
Climate change is constantly raising temperatures and increasing the frequency, duration, and intensity of heat waves, leading to various adverse health outcomes. The distribution of the above-mentioned impacts is not fair, and some individuals and groups are particularly affected. It is necessary to develop intervention strategies and policies targeting specific locations and populations to minimize the impact of high temperatures on health.
Post time: Aug-03-2024