Chronic lead poisoning is a significant risk factor for cardiovascular disease in adults and cognitive impairment in children, and can cause harm even at lead levels previously considered safe. In 2019, lead exposure was responsible for 5.5 million deaths from cardiovascular disease worldwide and a total loss of 765 million IQ points in children each year.
Lead exposure is almost everywhere, including in leaded paint, leaded gasoline, some water pipes, ceramics, cosmetics, fragrances, as well as smelting, battery production and other industries, so population-level strategies are important to eliminate lead poisoning.
Lead poisoning is an ancient disease. Dioscorides, a Greek physician and pharmacologist in ancient Rome, wrote De
Materia Medica, the most important work on pharmacology for decades, described the symptoms of overt lead poisoning nearly 2,000 years ago. People with overt lead poisoning experience fatigue, headache, irritability, severe abdominal cramps, and constipation. When the blood lead concentration exceeds 800 μg/L, acute lead poisoning can cause convulsions, encephalopathy, and death.
Chronic lead poisoning was recognized more than a century ago as a cause of atherosclerosis and “lead toxic” gout. At autopsy, 69 of 107 patients with lead-induced gout had “hardening of the artery wall with atheromatous changes.” In 1912, William Osler (William Osler)
“Alcohol, lead, and gout play important roles in the pathogenesis of arteriosclerosis, although the exact modes of action are not well understood,” Osler wrote. The lead line (a fine blue deposit of lead sulfide along the edge of the gums) is characteristic of chronic lead poisoning in adults.
In 1924, New Jersey, Philadelphia and New York City banned the sale of leaded gasoline after 80 percent of workers producing tetraethyl lead at Standard Oil in New Jersey were found to have lead poisoning, some of whom died. On May 20, 1925, Hugh Cumming, the surgeon general of the United States, convened scientists and industry representatives to determine whether it was safe to add tetraethyl lead to gasoline. Yandell Henderson, a physiologist and expert in chemical warfare, warned that “the addition of tetraethyl lead will slowly expose a large population to lead poisoning and hardening of the arteries”. Robert Kehoe, chief medical officer of Ethyl Corporation, believes government agencies should not ban tetraethyl lead from cars until it has been proven toxic. “The question is not whether lead is dangerous, but whether a certain concentration of lead is dangerous,” Kehoe said.
Although lead mining has been going on for 6,000 years, lead processing increased dramatically in the 20th century. Lead is a malleable, durable metal used to prevent fuel from burning too fast, reduce “engine knock” in cars, transport drinking water, solder food cans, make paint shine long and kill insects. Unfortunately, most of the lead used for these purposes ends up in people’s bodies. At the peak of the lead poisoning epidemic in the United States, hundreds of children were hospitalized each summer for lead encephalopathy, and a quarter of them died.
Humans are currently exposed to lead at levels well above natural background levels. In the 1960s, geochemist Clair Patterson, who used lead isotopes to estimate the age of the Earth at 4.5 billion years
Patterson found that mining, smelting and vehicle emissions resulted in atmospheric lead deposits 1,000 times higher than natural background levels in glacier core samples. Patterson also found that the concentration of lead in the bones of people in industrialized countries was 1,000 times higher than that of people living in pre-industrial times.
Lead exposure has declined by more than 95% since the 1970s, but the current generation still carries 10-100 times more lead than people living in pre-industrial times.
With a few exceptions, such as lead in aviation fuel and ammunition and lead-acid batteries for motor vehicles, lead is no longer used in the United States and Europe. Many doctors believe the problem of lead poisoning is a thing of the past. However, lead paint in older homes, leaded gasoline deposited in the soil, lead leached from water pipes, and emissions from industrial plants and incinerators all contribute to lead exposure. In many countries, lead is emitted from smelting, battery production and e-waste, and is often found in paints, ceramics, cosmetics and fragrances. Research confirms that chronic low-level lead poisoning is a risk factor for cardiovascular disease in adults and cognitive impairment in children, even at levels previously considered safe or harmless. This article will summarize the effects of chronic low-level lead poisoning
Exposure, absorption and internal load
Oral ingestion and inhalation are the main routes of lead exposure. Infants with rapid growth and development can easily absorb lead, and iron deficiency or calcium deficiency can promote lead absorption. Lead mimicking calcium, iron, and zinc enters the cell through calcium channels and metal transporters such as divalent metal transporter 1[DMT1]. People with genetic polymorphisms that promote iron or calcium absorption, such as those that cause hemochromatosis, have increased lead absorption.
Once absorbed, 95% of the residual lead in an adult’s body is stored in the bones; 70% of residual lead in a child’s body is stored in the bones. About 1% of the total lead load in the human body circulates in the blood. 99% of the lead in the blood is in the red blood cells. Whole blood lead concentration (newly absorbed lead and remobilized lead from bone) is the most widely used biomarker of exposure level. Factors that alter bone metabolism, such as menopause and hyperthyroidism, can release lead sequestrated in the bones, causing blood lead levels to spike.
In 1975, when lead was still being added to gasoline, Pat Barry conducted an autopsy study of 129 British people and quantified their total lead load. The average total load in a man’s body is 165 mg, equivalent to the weight of a paper clip. The body load of the men with lead poisoning was 566 mg, only three times the average load of the entire male sample. In comparison, the average total load in a woman’s body is 104 mg. In both men and women, the highest concentration of lead in soft tissue was in the aorta, while in men the concentration was higher in atherosclerotic plaques.
Some populations are at increased risk of lead poisoning compared to the general population. Infants and young children are at greater risk of ingesting lead because of their non-eating oral behavior, and they are more likely to absorb lead than older children and adults. Young children living in poorly maintained homes built before 1960 are at risk of lead poisoning from ingesting paint chips and lead-contaminated house dust. People who drink tap water from lead-contaminated pipes or live near airports or other lead-contaminated sites are also at increased risk of developing low-level lead poisoning. In the United States, lead concentrations in the air are significantly higher in segregated communities than in integrated communities. Workers in the smelting, battery recycling and construction industries, as well as those who use firearms or have bullet fragments in their bodies, are also at increased risk of lead poisoning.
Lead is the first toxic chemical measured in the National Health and Nutrition Examination Survey (NHANES). At the beginning of the phase-out of leaded gasoline, blood lead levels plummeted from 150 μg/L in 1976 to 90 in 1980
μg/L, a symbolic number. Blood lead levels deemed potentially harmful have been lowered several times. In 2012, the Centers for Disease Control and Prevention (CDC) announced that a safe level of lead in children’s blood has not been determined. The CDC lowered the standard for excessive blood lead levels in children – often used to indicate that action should be taken to reduce lead exposure – from 100 μg/L to 50 μg/L in 2012, and to 35 μg/L in 2021. The lowering of the standard for excessive blood lead influenced our decision that this paper will use μg/L as a unit of measurement for blood lead levels, rather than the more commonly used μg/dL, which reflects the extensive evidence of lead toxicity at lower levels.
Death, illness and disability
“Lead is potentially toxic anywhere, and lead is everywhere,” wrote Paul Mushak and Annemarie F. Crocetti, both members of the National Board of Air Quality appointed by President Jimmy Carter, in a report to Congress in 1988. The ability to measure lead levels in blood, teeth and bones reveals a range of medical problems associated with chronic low-level lead poisoning at the levels commonly found in the human body. Low levels of lead poisoning are a risk factor for preterm birth, as well as cognitive impairment and attention deficit hyperactivity disorder (ADHD), increased blood pressure and reduced heart rate variability in children. In adults, low levels of lead poisoning are a risk factor for chronic kidney failure, hypertension and cardiovascular disease
Growth and neurodevelopment
At concentrations of lead commonly found in pregnant women, lead exposure is a risk factor for preterm birth. In a prospective Canadian birth cohort, a 10 μg/L increase in maternal blood lead levels was associated with a 70% increased risk of spontaneous preterm birth. For pregnant women with serum vitamin D levels below 50 mmol/L and blood lead levels increased by 10 μg/L, the risk of spontaneous preterm birth increased to three times.
In an earlier landmark study of children with clinical signs of lead poisoning, Needleman et al. found that children with higher levels of lead were more likely to develop neuropsychological deficits than children with lower levels of lead, And were more likely to be rated as poor by teachers in areas such as distraction, organizational skills, impulsivity and other behavioral traits. Ten years later, children in the group with higher dentin lead levels were 5.8 times more likely to have dyslexia and 7.4 times more likely to drop out of school than children in the group with lower lead levels.
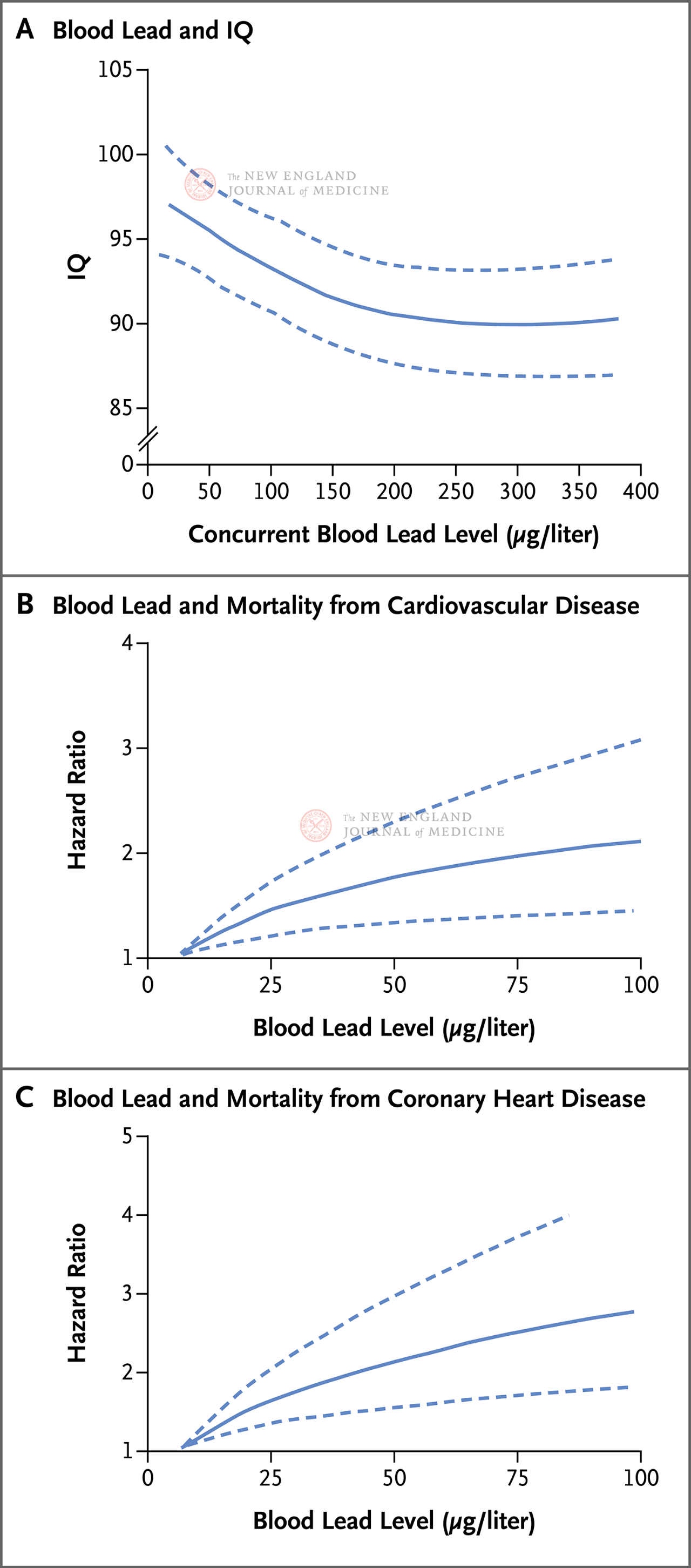
The ratio of cognitive decline to increase in lead levels was greater in children with low lead levels. In a pooled analysis of seven prospective cohorts, an increase in blood lead levels from 10 μg/L to 300 μg/L was associated with a 9-point decrease in children’s IQ, but the largest decrease (a 6-point decrease) occurred when blood lead levels first increased by 100 μg/L. Dose-response curves were similar for cognitive decline associated with measured lead levels in bone and plasma.
Lead exposure is a risk factor for behavioral disorders such as ADHD. In a nationally representative U.S. study of children ages 8 to 15, children with blood lead levels greater than 13 μg/L were twice as likely to have ADHD as those with blood lead levels in the lowest quintile. In these children, approximately 1 in 5 cases of ADHD can be attributed to lead exposure.
Childhood lead exposure is a risk factor for antisocial behavior, including behavior associated with conduct disorder, delinquency, and criminal behavior. In a meta-analysis of 16 studies, elevated blood lead levels were consistently associated with conduct disorder in children. In two prospective cohort studies, higher blood lead or dentin lead levels in childhood were associated with higher rates of delinquency and arrest in young adulthood.
Higher lead exposure in childhood was associated with reduced brain volume (possibly due to reduced neuron size and dendrite branching), and the reduced brain volume persisted into adulthood. In a study that included older adults, higher blood or bone lead levels were prospectively associated with accelerated cognitive decline, especially in those who carried the APOE4 allele. Early childhood lead exposure may be a risk factor for developing late-onset Alzheimer’s disease, but the evidence is unclear.
Nephropathy
Lead exposure is a risk factor for developing chronic kidney disease. The nephrotoxic effects of lead are manifested in the intranuclear inclusion bodies of proximal renal tubules, tubule interstitial fibrosis and chronic renal failure. Among those who participated in the NHANES survey between 1999 and 2006, adults with blood lead levels above 24 μg/L were 56% more likely to have a reduced glomerular filtration rate (<60 mL/[min·1.73 m2]) than those with blood lead levels below 11 μg/L. In a prospective cohort study, people with blood lead levels above 33 μg/L had a 49 percent higher risk of developing chronic kidney disease than those with lower blood lead levels.
Cardiovascular disease
Lead induced cellular changes are characteristic of high blood pressure and atherosclerosis. In laboratory studies, chronically low levels of lead exposure increase oxidative stress, reduce levels of bioactive nitric oxide, and induce vasoconstriction by activating protein kinase C, leading to persistent hypertension. Lead exposure inactivates nitric oxide, increases hydrogen peroxide formation, inhibits endothelial repair, impairs angiogenesis, promotes thrombosis, and leads to atherosclerosis (Figure 2).
An in vitro study showed that endothelial cells cultured in an environment with lead concentrations of 0.14 to 8.2 μg/L for 72 hours caused cell membrane damage (small tears or perforations observed by scanning electron microscopy). This study provides ultrastructural evidence that newly absorbed lead or lead re-entering the blood from bone may cause endothelial dysfunction, which is the earliest detectable change in the natural history of atherosclerotic lesions. In a cross-sectional analysis of a representative sample of adults with an average blood lead level of 27 μg/L and no history of cardiovascular disease, blood lead levels increased by 10%
At μg, the odds ratio for severe coronary artery calcification (i.e., Agatston score >400 with a score range of 0[0 indicating no calcification] and higher scores indicating greater calcification range) was 1.24 (95% confidence interval 1.01 to 1.53).
Lead exposure is a major risk factor for death from cardiovascular disease. Between 1988 and 1994, 14,000 American adults took part in the NHANES survey and were followed for 19 years, of which 4,422 died. One in five people die of coronary heart disease. After adjusting for other risk factors, increasing blood lead levels from the 10th percentile to the 90th percentile was associated with a doubling of the risk of death from coronary heart disease. The risk of cardiovascular disease and coronary heart disease death rises sharply when lead levels are below 50 μg/L, with no clear threshold (Figures 3B and 3C). Researchers believe that a quarter of a million premature cardiovascular deaths each year are due to chronic low-level lead poisoning. Of these, 185,000 died from coronary heart disease.
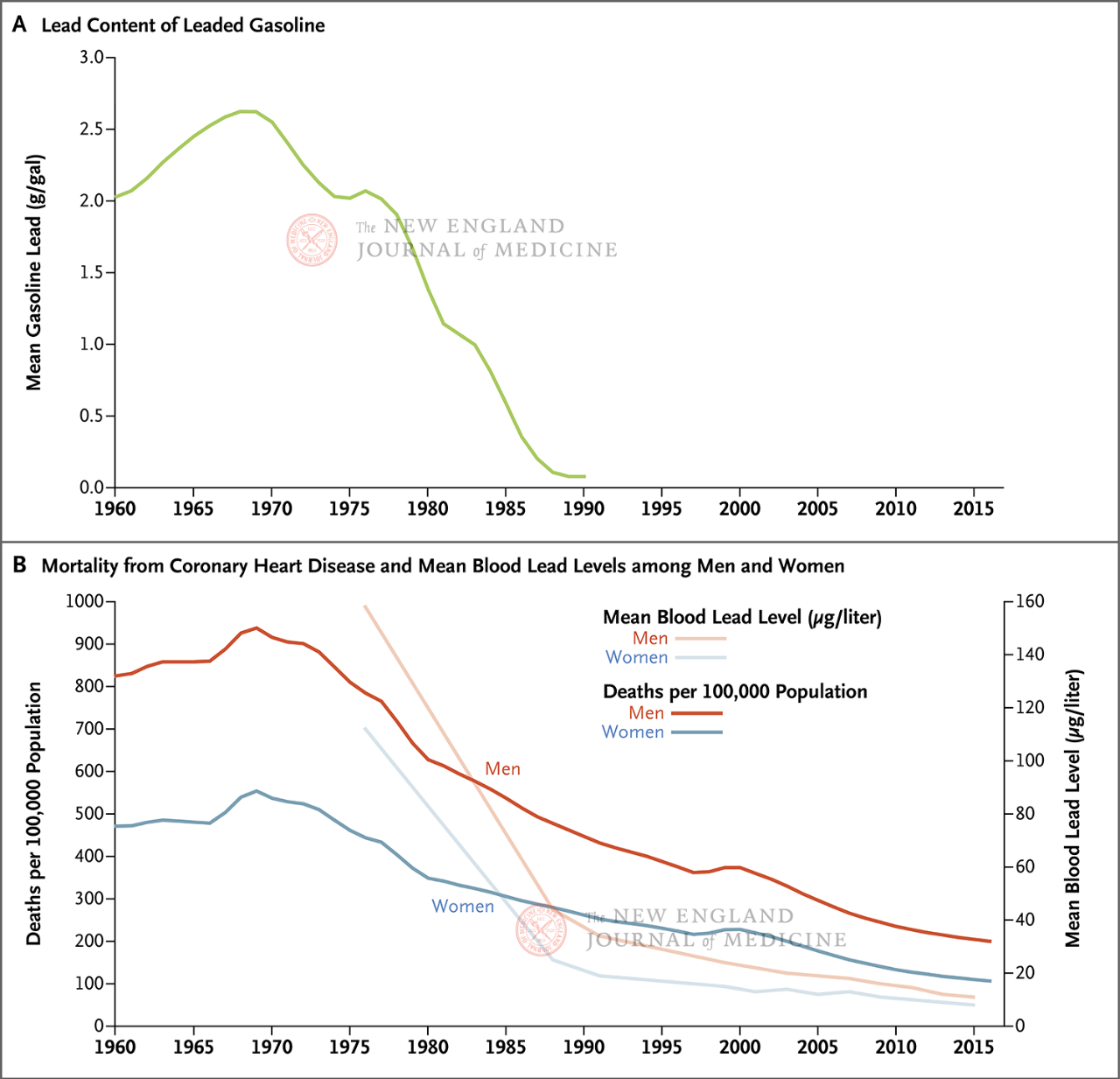
Lead exposure may be one of the reasons why coronary heart disease deaths first rose and then fell in the last century. In the United States, coronary heart disease death rates rose sharply in the first half of the 20th century, peaking in 1968, and then declining steadily. It is now 70 per cent below its 1968 peak. Lead exposure to leaded gasoline was associated with a decline in mortality from coronary heart disease (Figure 4). Among those who participated in the NHANES survey, which was followed for up to eight years between 1988-1994 and 1999-2004, 25% of the total reduction in coronary heart disease incidence was due to reduced blood lead levels.
In the early years of phasing out leaded gasoline, the incidence of high blood pressure in the United States dropped sharply. Between 1976 and 1980, 32 percent of American adults had high blood pressure. In 1988-1992, the proportion was only 20%. The usual factors (smoking, blood pressure medications, obesity, and even the larger size of the cuff used to measure blood pressure in obese people) do not explain the drop in blood pressure. However, the median blood lead level in the United States dropped from 130 μg/L in 1976 to 30 μg/L in 1994, suggesting that the decline in lead exposure is one reason for the drop in blood pressure. In the Strong Heart Family Study, which included an American Indian cohort, blood lead levels decreased by ≥9 μg/L and systolic blood pressure decreased by an average of 7.1 mm Hg (adjusted value).
Many questions remain unanswered about the effects of lead exposure on cardiovascular disease. The duration of exposure required to cause hypertension or cardiovascular disease is not fully understood, but long-term cumulative lead exposure measured in bone appears to have a stronger predictive power than short-term exposure measured in blood. However, reducing lead exposure appears to reduce blood pressure and the risk of death from cardiovascular disease within 1 to 2 years. A year after banning leaded fuel from NASCAR racing, communities near the track had significantly lower rates of coronary heart disease deaths compared with more peripheral communities. Finally, there is a need to study long-term cardiovascular effects in people exposed to lead levels below 10 μg/L.
Reduced exposure to other toxic chemicals also contributed to the decline in coronary heart disease. Phasing out leaded gasoline from 1980 to 2000 reduced particulate matter in 51 metropolitan areas, resulting in a 15 percent increase in life expectancy. Fewer people are smoking. In 1970, about 37 percent of American adults smoked; By 1990, only 25 percent of Americans smoked. Smokers have significantly higher blood lead levels than non-smokers. It is difficult to tease out the historical and current effects of air pollution, tobacco smoke and lead on coronary heart disease.
Coronary heart disease is the leading cause of death worldwide. More than a dozen studies have shown that lead exposure is a major and often overlooked risk factor for death from coronary heart disease. In a meta-analysis, Chowdhury et al found that elevated blood lead levels are an important risk factor for coronary heart disease. In eight prospective studies (with a total of 91,779 participants), people with blood lead concentrations in the highest quintile had an 85% higher risk of non-fatal myocardial infarction, bypass surgery, or death from coronary heart disease than those in the lowest quintile. In 2013, the Environmental Protection Agency (EPA)
The Protection Agency concluded that lead exposure is a risk factor for coronary heart disease; A decade later, the American Heart Association endorsed that conclusion.
Post time: Nov-02-2024