One hundred years ago, a 24-year-old man was admitted to Massachusetts General Hospital (MGH) with fever, cough, and difficulty breathing.
The patient had been healthy for three days before admission, then began to feel unwell, with general fatigue, headache and back pain. His condition worsened over the next two days and he spent most of his time in bed. One day before admission, he developed a high fever, dry cough and chills, which the patient described as “crouching” and completely unable to get out of bed. He took 648 mg of aspirin every four hours and experienced slight relief from headaches and back pain. However, on the day of admission, he came to the hospital after waking up in the morning with dyspnea, accompanied by subxiphoid chest pain, which was aggravated by deep breathing and coughing.
At admission, the rectal temperature was 39.5°C to 40.8°C, the heart rate was 92 to 145 beats/min, and the respiratory rate was 28 to 58 beats/min. The patient has a nervous and acute appearance. Though wrapped in multiple blankets, the chills continued. Shortness of breath, accompanied by paroxysms of intense cough, resulting in severe pain below the sternum, coughing up phlegm pink, viscous, slightly purulent.
Apical pulsation was palpable in the fifth intercostal space on the left side of the sternum, and no enlargement of the heart was observed on percussion. Auscultation revealed a rapid heart rate, consistent heart rhythm, audible at the apex of the heart, and a slight systolic murmur. Reduced breathing sounds on the right side of the back from one-third below the shoulder blades, but no rales or pleural fricatives were heard. Slight redness and swelling in the throat, tonsils removed. The scar of left inguinal hernia repair surgery is visible on the abdomen, and there is no swelling or tenderness in the abdomen. Dry skin, high skin temperature. The white blood cell count was between 3700 and 14500/ul, and neutrophils accounted for 79%. No bacterial growth was observed in blood culture.
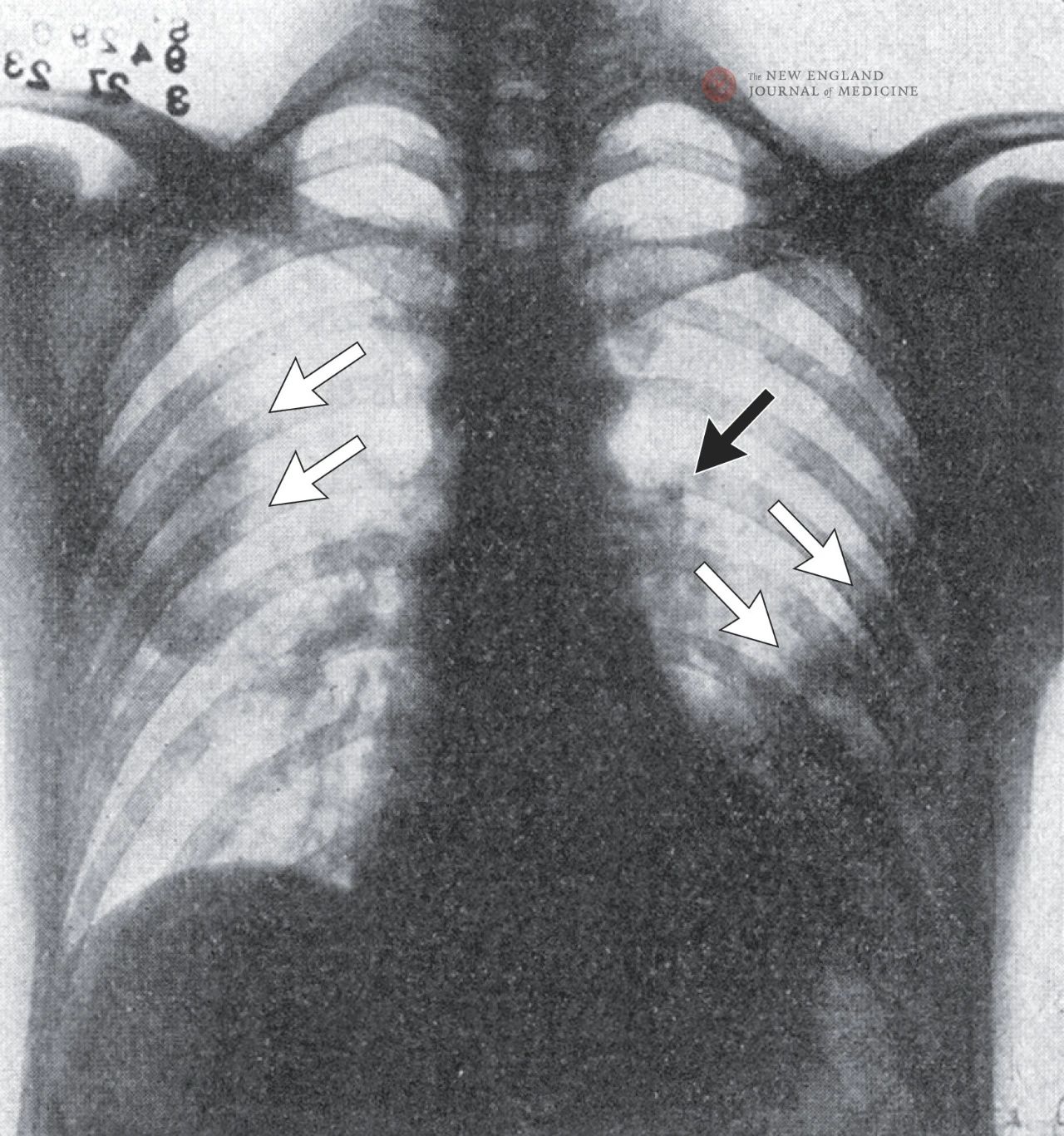
A chest radiograph shows patchy shadows on both sides of the lungs, particularly in the upper right lobe and lower left lobe, suggesting pneumonia. Enlargement of the left hilum of the lung suggests possible lymph node enlargement, with the exception of a left pleural effusion.
On the second day of hospitalization, the patient had dyspnea and persistent chest pain, and the sputum was purulent and bloodshot. Physical examination showed that there was systolic murmur conduction in the apex of the lung, and the percussion at the bottom of the right lung was dulled. Small, congested papules appear on the left palm and right index finger. Doctors described the patient’s condition as “grim”. On the third day, purulent sputum became more apparent. The dullness of the left lower back was enhanced while the tactile tremor was aggravated. Bronchial breathing sounds and a few rales can be heard on the left back one third of the way down from the shoulder blade. Percussion on the right back is slightly dulled, breathing sounds are distant, and occasional rales are audible.
On the fourth day, the patient’s condition deteriorated further and he died that night.
Diagnosis
The 24-year-old male was hospitalized in March 1923 with acute fever, chills, muscle soreness, shortness of breath, and pleurisy chest pain. His signs and symptoms are highly consistent with a respiratory viral infection, such as influenza, with possible secondary bacterial infection. Given that these symptoms are very similar to cases during the 1918 flu pandemic, influenza is probably the most reasonable diagnosis.
Although the clinical manifestations and complications of modern influenza closely resemble those of the 1918 pandemic, the scientific community has made important breakthroughs in the past few decades, including the identification and isolation of influenza viruses, the development of rapid diagnostic techniques, the introduction of effective antiviral treatments, and the implementation of surveillance systems and vaccination programs. Looking back at the 1918 flu pandemic not only reflects on the lessons of history, but also better prepares us for future pandemics.
The 1918 flu pandemic began in the United States. The first confirmed case occurred on March 4, 1918, in an Army cook at Fort Riley, Kansas. Then Lorrin Miner, a doctor in Haskell County, Kansas, documented 18 cases of severe flu, including three deaths. He reported this finding to the US Department of Public Health, but it was not taken seriously.
Historians believe that the failure of the public health authorities at the time to respond to the outbreak was closely related to the special context of the First World War. To avoid affecting the course of the war, the government kept quiet about the severity of the outbreak. John Barry, author of The Great Flu, criticized the phenomenon in a 2020 interview: “The government is lying, they’re calling it the common cold, and they’re not telling the public the truth.” In contrast, Spain, a neutral country at the time, was the first to report the flu in the media, leading to the new viral infection being named “Spanish flu,” even though the earliest cases were recorded in the United States.
Between September and December 1918, an estimated 300,000 people died of influenza in the United States, 10 times the number of deaths from all causes in the United States during the same period in 1915. Flu spreads rapidly through military deployments and personnel movements. Soldiers not only moved between transport hubs in the east, but also carried the virus to the battlefields of Europe, spreading the flu around the world. It is estimated that more than 500 million people have been infected and about 100 million have lost their lives.
Medical treatment was extremely limited. Treatment is primarily palliative, including the use of aspirin and opiates. The only treatment that is likely to be effective is convalescent plasma infusion – known today as convalescent plasma therapy. However, flu vaccines have been slow to arrive because scientists have yet to identify the cause of the flu. In addition, more than a third of American doctors and nurses have been removed because of their involvement in the war, leaving medical resources even more scarce. Although vaccines were available for cholera, typhoid, plague, and smallpox, the development of an influenza vaccine was still lacking.
Through the painful lessons of the 1918 influenza pandemic, we learned the importance of transparent information disclosure, the advancement of scientific research, and cooperation in global health. These experiences provide valuable insights for addressing similar global health threats in the future.
Virus
For many years, the causative agent of the “Spanish flu” was thought to be the bacterium Pfeiffer (now known as Haemophilus influenzae), which was found in the sputum of many, but not all, patients. However, this bacterium is considered difficult to culture due to its high culture conditions, and because it has not been seen in all cases, the scientific community has always questioned its role as a pathogen. Subsequent studies have shown that Haemophilus influenzae is actually the pathogen of a bacterial double infection common in influenza, rather than the virus that directly causes influenza.
In 1933, Wilson Smith and his team made a breakthrough. They took samples from pharyngeal flusher from flu patients, ran them through a bacterial filter to eliminate bacteria, and then experimented with the sterile filtrate on ferrets. After an incubation period of two days, the exposed ferrets began to show symptoms similar to human influenza. The study is the first to confirm that influenza is caused by viruses rather than bacteria. In reporting these findings, the researchers also noted that previous infection with the virus can effectively prevent re-infection of the same virus, which lays the theoretical basis for vaccine development.
A few years later, Smith’s colleague Charles Stuart-Harris, while observing a ferret infected with influenza, accidentally contracted the virus from close exposure to the ferret’s sneeze. The virus isolated from Harris then successfully infected an uninfected ferret, reaffirming the ability of influenza viruses to spread between humans and animals. In a related report, the authors noted that “it is conceivable that laboratory infections could be the starting point for epidemics.”
Vaccine
Once the flu virus was isolated and identified, the scientific community quickly began developing a vaccine. In 1936, Frank Macfarlane Burnet first demonstrated that influenza viruses could grow efficiently in fertilized eggs, a discovery that provided a breakthrough technology for vaccine production that is still widely used today. In 1940, Thomas Francis and Jonas Salk successfully developed the first flu vaccine.
The need for a vaccine was particularly pressing for the U.S. military, given the devastating impact of influenza on U.S. troops during World War I. In the early 1940s, U.S. Army soldiers were among the first to receive the flu vaccine. By 1942, studies confirmed that the vaccine was effective in providing protection, and vaccinated people were significantly less likely to contract the flu. In 1946, the first flu vaccine was approved for civilian use, opening a new chapter in flu prevention and control.
It turns out that getting the flu vaccine has a significant effect: unvaccinated people are 10 to 25 times more likely to get the flu than those who do.
Surveillance
Influenza surveillance and its specific virus strains are essential to guide public health responses and develop vaccination schedules. Given the global nature of influenza, national and international surveillance systems are particularly necessary.
The Centers for Disease Control and Prevention (CDC) was founded in 1946 and initially focused on research into disease outbreaks such as malaria, typhus and smallpox. Within five years of its creation, CDC created the Epidemic Intelligence Service to provide specialized training to investigate disease outbreaks. In 1954, the CDC established its first influenza surveillance system and began issuing regular reports on influenza activity, laying the foundation for influenza prevention and control.
At the international level, the World Health Organization (WHO) established the Global Influenza Surveillance and Response System in 1952, working closely with the Global Sharing of Influenza Data Initiative (GISAID) to form a global influenza surveillance system. In 1956, the WHO further designated CDC as its collaborating center in the field of influenza surveillance, epidemiology and control, providing technical support and scientific guidance for global influenza prevention and control. The establishment and continued operation of these surveillance systems provides an important safeguard for the global response to influenza epidemics and pandemics.
At present, the CDC has established an extensive domestic influenza surveillance network. The four core components of influenza surveillance include laboratory testing, out-patient case surveillance, in-patient case surveillance, and death surveillance. This integrated surveillance system provides important support to guide public health decision-making and response to an influenza pandemic .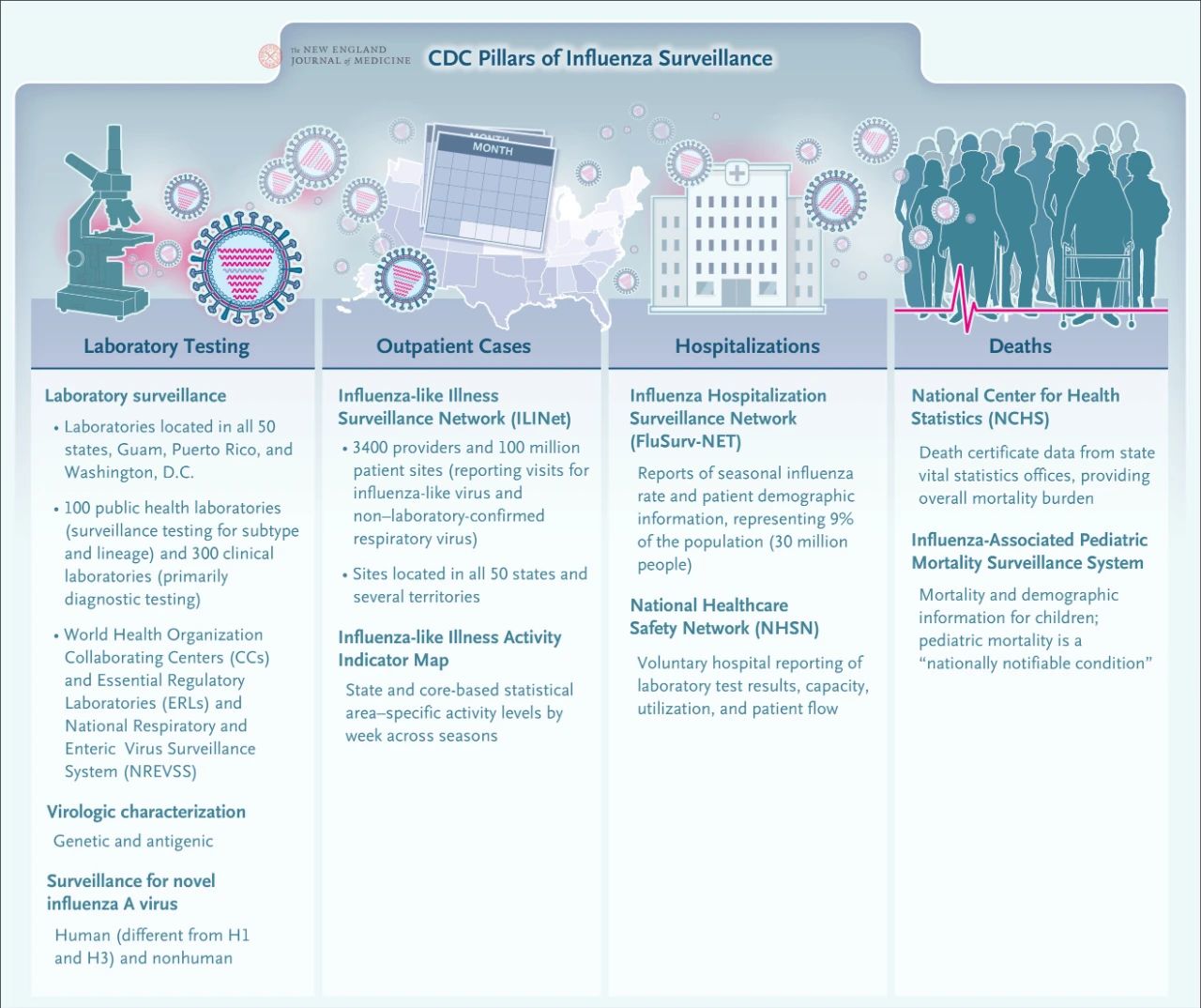
The Global Influenza Surveillance and Response System covers 114 countries and has 144 national influenza centres, which are responsible for continuous influenza surveillance throughout the year. The CDC, as a member, works with laboratories in other countries to send influenza virus isolates to the WHO for antigenic and genetic profiling, similar to the process by which U.S. laboratories submit isolates to the CDC. The cooperation between the United States and China over the past 40 years has become an important part of global health security and diplomacy.
Post time: Dec-21-2024