The study found that in the age group 50 years and older, lower socioeconomic status was significantly associated with an increased risk of depression; Among them, low participation in social activities and loneliness play a mediating role in the causal association between the two. The research results reveal for the first time the mechanism of action between psychosocial behavioral factors and socio-economic status and the risk of depression in the elderly, and provide important scientific evidence support for the formulation of comprehensive mental health interventions in the elderly population, the elimination of social determinants of health, and the acceleration of the realization of global healthy aging goals
Depression is the leading mental health problem contributing to the global burden of disease and the leading cause of death among mental health problems. The Comprehensive Action Plan for Mental Health 2013-2030, adopted by WHO in 2013, highlights key steps to provide appropriate interventions for people with mental disorders, including those with depression. Depression is prevalent in the elderly population, but it is largely undiagnosed and untreated. Studies have found that depression in old age is strongly associated with cognitive decline and the risk of cardiovascular disease. Socioeconomic status, social activity, and loneliness have been independently associated with the development of depression, but their combined effects and specific mechanisms are unclear. In the context of global aging, there is an urgent need to clarify the social health determinants of depression in old age and their mechanisms.
This Study is a population-based, cross-country cohort study using data from five nationally representative surveys of older adults in 24 countries (conducted from February 15, 2008 to February 27, 2019), including the Health and Retirement Study, a national Health and Retirement Study. HRS, the English Longitudinal Study of Ageing, ELSA, the Survey of Health, Ageing and Retirement in Europe, The Survey of Health, Ageing and Retirement in Europe, the China Health and Retirement Longitudinal Study, The China Health and Retirement Longitudinal Study, CHARLS and the Mexican Health and Ageing Study (MHAS). The study included participants aged 50 years and older at baseline who reported information on their socioeconomic status, social activities, and feelings of loneliness, and who were interviewed at least twice; Participants who had depressive symptoms at baseline, those who were missing data on depressive symptoms and covariates, and those who were missing were excluded. Based on household income, education and employment status, the underlying category analysis method was used to define socioeconomic status as high and low. Depression was assessed using the Mexican Health and Ageing Study (CES-D) or EURO-D. The association between socioeconomic status and depression was estimated using the Cox proportional hazard model, and the pooled results of five surveys were obtained using a random effects model. This study further analyzed the joint and interactive effects of socioeconomic status, social activities and loneliness on depression, and explored the mediating effects of social activities and loneliness on socioeconomic status and depression by using causal mediation analysis.
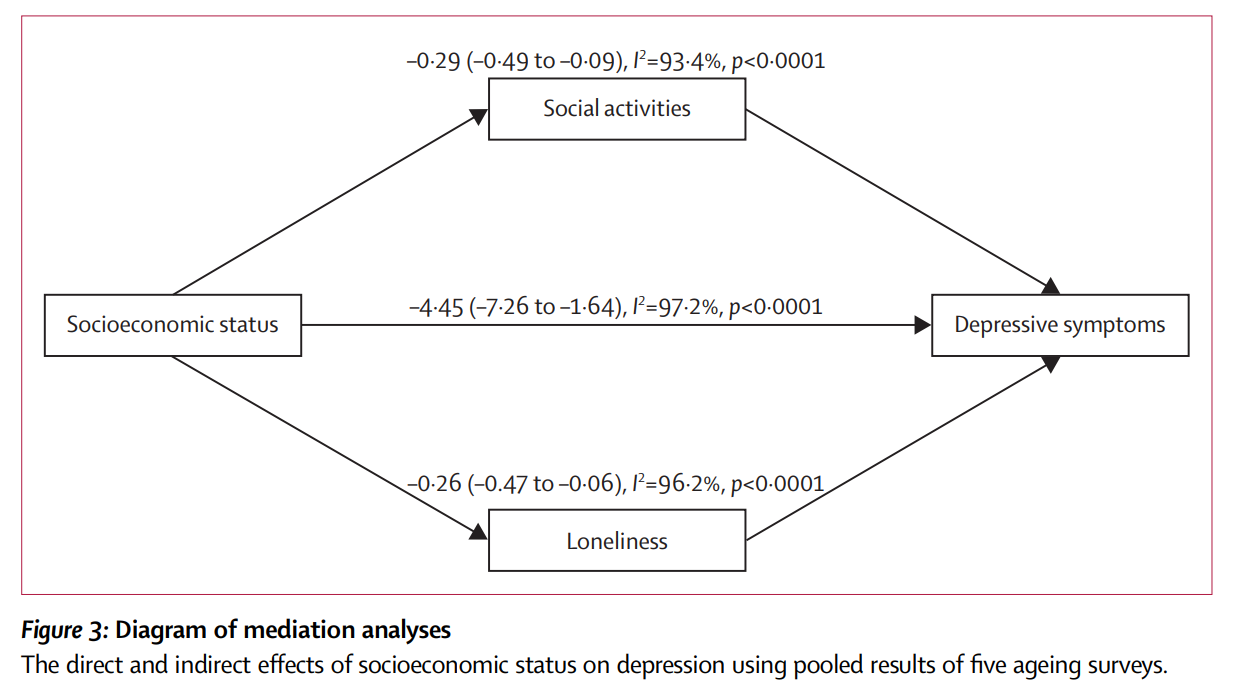
After a median follow-up of 5 years, 20,237 participants developed depression, with an incidence rate of 7.2 (95% confidence interval 4.4-10.0) per 100 person-years. After adjusting for a variety of confounding factors, the analysis found that participants of lower socioeconomic status had a higher risk of depression compared to participants of higher socioeconomic status (pooled HR=1.34; 95% CI: 1.23-1.44). Of the associations between socioeconomic status and depression, only 6.12% (1.14-28.45) and 5.54% (0.71-27.62) were mediated by social activities and loneliness, respectively.
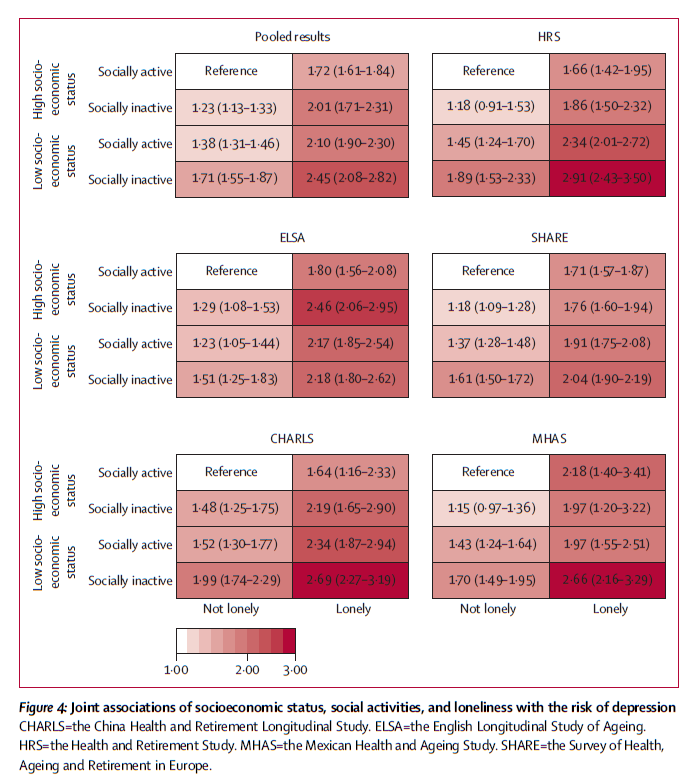
Only the interaction between socioeconomic status and loneliness was observed to have a significant effect on depression (pooled HR=0.84; 0.79-0.90). Compared with participants of high socioeconomic status who were socially active and not lonely, participants of low socioeconomic status who were socially inactive and lonely had a higher risk of depression (aggregate HR=2.45;2.08-2.82).
Social passivity and loneliness only partially mediate the association between socioeconomic status and depression, suggesting that in addition to interventions targeting social isolation and loneliness, other effective measures are needed to reduce the risk of depression in older adults. Furthermore, the combined effects of socioeconomic status, social activity, and loneliness highlight the benefits of simultaneous integrated interventions to reduce the global burden of depression.
Post time: Sep-07-2024